Contemplating Contraceptives with the Student Health Educators
What comes to mind when you hear the word “contraception”? Do you think of a condom or a pack of little pink pills? Both are popular methods of birth control, but there’s actually a whole lot out there in terms of ways to prevent pregnancy. If you are sexually active or planning on being sexually active at some point, it’s worthwhile to explore every option and become familiar with how they work. Individuals choose different methods for a variety of reasons: cost, potential side effects, level of comfort with one’s body, effectiveness in preventing pregnancy, effectiveness in preventing S.T.I transmission and frequency of sexual activity.
Navigating the world of contraceptive methods can get confusing, but luckily, the Student Health Educators are here to help! (Disclaimer: this article focuses on ways to prevent pregnancy. If that’s not an issue for you and your partner, it’s still important to protect yourself against S.T.I.’s — use barrier methods such as condoms and dental dams!)
First, let’s start with our old friend: the condom. You’ve seen condoms during your first-year orientation skits and in little bowls in dorm bathrooms, but how effective are they in preventing pregnancy? When used correctly, condoms are 99 percent effective, however, actual user effectiveness (meaning the effectiveness of typical use — accounting for improper application, tearing or slippage) is a much lower 86 percent. Using spermicide or a condom with spermicidal lubricant can provide additional protection. Condoms can be used as a primary, supplemental or back-up method of birth control.
PROS: Protect against both pregnancy and S.T.I. transmission, can find them over-the-counter or FREE from your RCs!
CONS: Not as effective as some other forms of contraception.
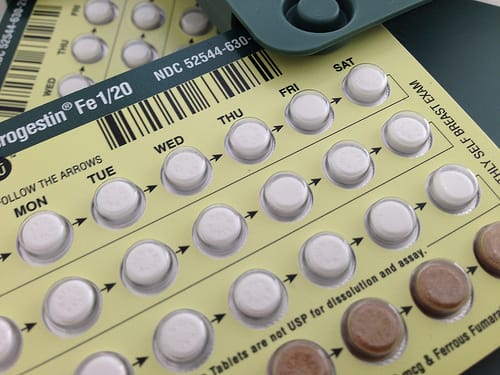
Let’s move on to forms of oral contraceptives — “the pill.” As a hormonal contraceptive, the pill releases a synthetic combination of the hormones estrogen and progestin. This contraceptive helps your body maintain a constant hormone level throughout the month, which inhibits ovulation. Most oral contraceptives come in 28-pill packages with seven sugar pills that initiate menstruation. Although it requires a prescription, it’s easy to ask for one at the health center, and it’s confidential. The pill is popular for good reason — it’s 99.7 percent effective when used perfectly. “Perfect” use means taking the pill at or around the same time every day to maintain the correct hormonal balance and avoiding any antibiotics that could interfere with efficacy. Remembering to take the pill at the same time every day isn’t always easy to do, which is why the effectiveness for actual use is 92 percent, accounting for forgetting or skipping pills. You’ll still be protected if you miss one pill, as long as you take it as soon as you remember and use a back-up method of birth control. If you miss more than two pills, you will not be fully protected and will need to start a new pack. If you have problems remembering to take the pill, try setting a daily alarm or downloading one of the many pill-reminder apps.
PROS: Very effective if taken diligently, most insurance covers it (thanks, Obama!).
CONS: Easy to forget a pill, requires a prescription.
If you just can’t seem to remember to take a pill, or if it just seems like a hassle, there are plenty of options that are just as effective. A contraceptive vaginal ring, better known as NuvaRing, is a flexible ring that is easily inserted into the vagina and releases a low dose of estrogen and progestin. The ring is kept in for three weeks and taken out on the fourth week to initiate the menstrual cycle. NuvaRing has the same high effectiveness as oral contraceptives, but if the ring is taken out for more than three hours a back-up method is recommended. Most women say they can’t feel the ring once it is in place and neither can their partner.
PROS: Don’t have to remember to take a pill every day.
CONS: Can be expensive without medical coverage.
Another option for those who want to forgo the pill is the “patch”: a thin, beige patch that attaches to the skin and releases hormones similarly to oral contraceptives. Just like NuvaRing, it’s used for three consecutive weeks and taken off on the fourth week. And just like the other hormonal contraceptives (the pill and NuvaRing), it’s highly effective! The patch adherence is high — heat, humidity, showering or exercise won’t cause it to come off.
PROS: Don’t have to remember to take a pill every day.
CONS: Depending on where you choose to put it, patch can be visible to others.
One of the most highly effective methods of contraception (with an actual effectiveness of 99.8 percent) is the Intrauterine Device, or IUD. An IUD is a small T-shaped device made of copper or plastic that is inserted and placed against the cervix by a health care provider. The two main IUD options are the copper IUD, which impairs sperm function, and the levonorgestrel IUD, which inhibits sperm survival by releasing a hormone in low doses. The levonorgestrel IUD lasts five to seven years, and the copper IUD lasts 10 to 12 years.
PROS: Highly effective, don’t have to remember to take a pill every day, available nearby at the Hadley Women’s Center and at UMass Health Services.
CONS: Expensive — cost ranges from $600 to $1200.
Lastly, in the case of unprotected intercourse or a failure in birth control, such as a broken condom, Plan B otherwise known as the “morning-after pill” is available at Amherst College Health center or over-the-counter at Target, CVS or Wal-Mart. This pill will delay ovulation, prevent fertilization or inhibit an already fertilized egg if used within 120 hours (five days) after unprotected sex. It has higher effectiveness in the first 72 hours, so the sooner you take it, the better. Plan B reduces the risk of pregnancy by 74 to 89 percent. It’s available for $35 after a visit with an Amherst College clinician, but it’s about two to three times more expensive purchased over the counter. It can be a good idea to purchase a pack in advance, in case of emergency or a friend’s emergency.
Making a decision about contraception really comes down to knowing your habits and level of comfort. It can take trial and error to find the best form of birth control for you. Plus, it doesn’t always have to do with sex — plenty of women choose to use birth control because for skin benefits, reduced menstrual cramps or the convenience of having a regulated menstrual cycle. But if you are engaging in sexual activity, it’s important to protect against S.T.I.’s as well as pregnancy by using condoms. A conversation between partners about birth control methods is important before engaging in any type of sexual activity where pregnancy or S.T.I. transmission is a risk. Have fun, be safe and if you have any questions, the Health Center staff and the SHEs are here to help.

Comments ()