Thoughts on Theses: Christine Kim
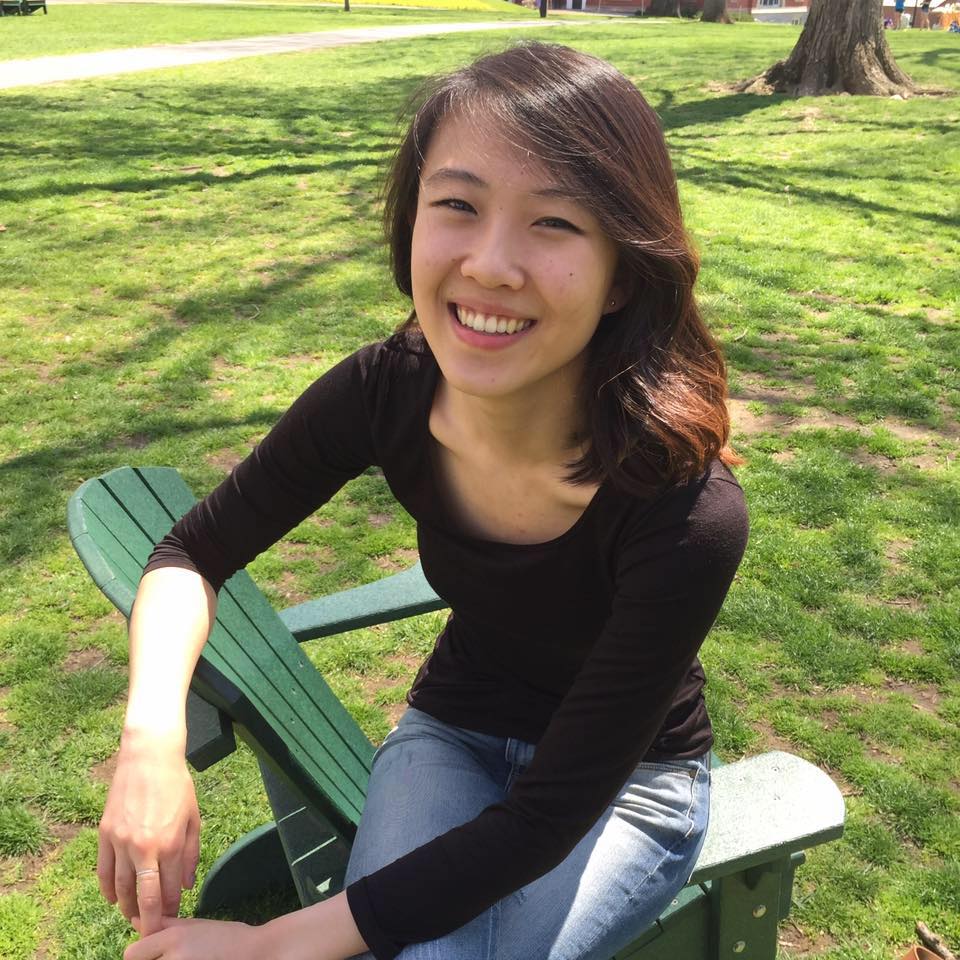
Christine Kim ’18 is an interdisciplinary major. Her thesis, titled “The Role of Medical Humanities in U.S. Education,” explores the evolving role that humanities play in medical school education. Her advisers are Professor of History John W. Servos, Professor of the History of Art and Asian Languages and Civilizations Samuel C. Morse and Health Professions Advisor Richard A. Aronson.
Q: What does it mean to be an interdisciplinary major?
A: Many people don’t realize that being an interdisciplinary major is even an option. I was originally an art history major until I spoke at length with my residential counselor at the time, who was an interdisciplinary major himself. He convinced me to become an interdisciplinary major. While it comes with certain requirements, such as having to take at least six relevant courses that you choose and having to write a thesis, I certainly think it’s a rewarding experience.
Q: How does the subject of medical humanities contribute to your thesis?
A: It’s certainly a broad topic. It’s a topic that has been around since around the 1970s and is a heavily researched topic. Medical humanities describes the intersection of humanities in medical education. I decided to narrow the topic down to U.S. medical schools. Basically, I’m looking at medical schools as educational institutions and exploring the role of humanities and how they play into the training of doctors.
Q: How do you plan on approaching this topic?
A: I was convinced that the best way to approach this would be to do interviews of students and faculty at U.S. medical schools and analyze the social and cultural challenges that the humanities departments at medical schools face. To get a well-rounded understanding, I plan on interviewing 10 students and faculty involved in medical schools with humanities departments and 10 students and faculty that are not involved in humanities in their medical schools. The background here is a movement that started about 50 years ago of attempting to produce more humane doctors: exploring exactly what it meant to be a humane doctor and more importantly, teaching medical students how best to communicate with future patients. However, this movement has not yet been entirely incorporated into medical school curricula. It was only just recently, for example, that they added social sciences to the MCAT [Medical College Admissions Test]. This step has been long anticipated. Many doctors give lip service to being more humanistic, caring, compassionate and being good listeners, but the fact that we live in a biologically-centered Western society gets in the way of including the humanities in medical school education. Because of this, I plan on interviewing current faculty and students, but also reviewing historical literature concerning this movement.
Q: How do you think the Western focus on the biological disrupts this incorporation?
A: It has a lot to do with the history of how medical schools were set up. Most medical schools in the U.S. still feel the impact of the Flexner report [a book-length study on recommendations for medical school reform published in 1910]. Flexner’s report revolutionized how medical schools taught and selected students — and it revolved around research. It made the push to turn medical schools and hospitals into research hubs. The social, cultural and political context of the U.S. at the time facilitated his recommendations coming to fruition. However, we are seeing a harder time bringing humanities in lockstep with contemporary medical school curricula even though this incorporation would further their goal of producing better doctors — likely because of our overwhelming focus on the biological that ignores the many contributions that the social sciences and the humanities can and have played in advancing medical outcomes. Crucially, medical schools tend to follow trends in general education as a whole, mainly because they themselves are educational institutions as as well. The general vogue in higher education has been including more STEM [science, technology, engineering and mathematics] classes and less humanities, and medical schools have similarly followed suit.
Q: What do you think are the consequences of not including enough humanities in U.S. medical curriculum?
A: We lose an opportunity to sharpen an important skill in the medicine: communication. While it’s true you are treating disease as a doctor, you are interacting with people, and people of different backgrounds view or perceive disease and medicine differently through different cultural lenses. The humanities in medical training provide an important opportunity to improve the cultural sensitivity of future physicians and to provide a crucial awareness of how medicine is looked at and approached differently by those of different backgrounds.
Q: What inspired you to pursue this thesis?
A: I came to Amherst as a pre-med student not really knowing what doctors do in real life. I had no idea what it was like to be a doctor on a day-to-day basis. I took the courses I needed for pre-med, but not really caring that much … because I lacked the passion for it. I feel as if I did it for the sake of doing it. Between sophomore and junior year, however, I took a gap year to work as a paramedic in Cambridge — that is what interested me in EMS [emergency medical services]. I went to paramedic school, and that allowed me to get clinical exposure. I also did clinical research at the oncology unit at a hospital and got a different exposure in the sense that I was now part of the hospital “system,” rather than simply field experience. However, I was pretty disappointed by my time at the hospital. We often have ideas about what the medical system is or ought to be, and I think more often than not our medical system disappoints the individuals it intends to serve. My experience as a paramedic and a researcher helped show me many of the ways in which our medical system fails us. Seeing how our medical system is broken helped me to start asking questions about why doctors face such challenges delivering proper care under this system. Also, like I said, before I took a gap year I was an art history major, and I had a conversation at the time with a professor from Harvard who takes medical students to art museums and teaches them how to formally critique art. He did a study that showed something like a 30 percent increase in correct diagnostic skills after teaching medical students such skills. These experiences were the inspiration behind my thesis.
Q: What classes helped you develop your idea for this thesis?
A: I kept seeing patterns in many of my classes. In particular was “Social Class” by Professor [of Sociology Ron] Lembo, which encouraged me to do interviews on top of simply literature review. His class in particular taught me the value of interviewing and how there is only so much that can be learned through literature without confronting the actual lived experiences of individuals in real life.


Comments ()